Panuveitis involves inflammation inside the eye that similarly affects the front, middle and back of the eye. It may be associated with any of the symptoms described in the other types of uveitis.
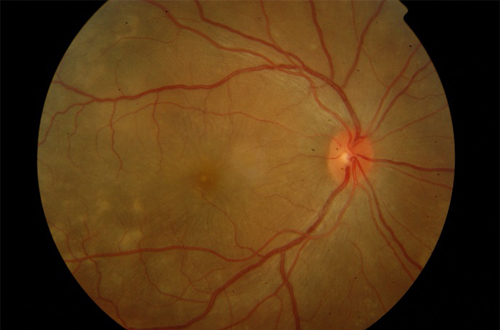
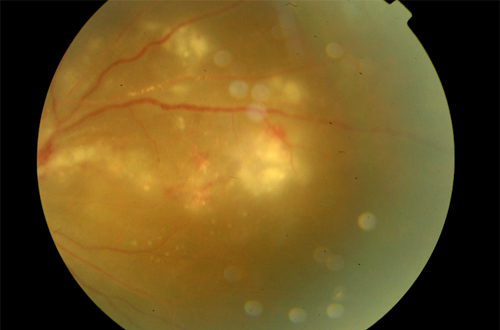
Because of the continuity between the various parts of the uvea, aqueous humor, and vitreous, however, uveal inflammation often involves many ocular structures. The retina and choroid are adjacent, with no major barriers between, so they are frequently inflamed together.
Clinical signs more specific for uveitis are as follows:
- Aqueous flare
- Inflammatory cells free in the anterior
- chamber or adherent to the corneal
- endothelium (keratic precipitates)
- Hypopyon or hyphema
- Episcleral vascular injection or
- circumcorneal ciliary flush
- Corneal edema
- Miosis
- Resistance to mydriatics
- Lowered IOP
- Anterior or posterior synechiae
- Swollen or dull appearance of the iris
- Increased pigmentation of the iris
- Vitreous haze or opacity
- Retinal edema, exudate, or detachment
- Aqueous lipemia, which may be seen if
- circulating lipid levels are high.